Introduction:
Hematologic malignancies (HM) are a diverse group of blood cancers with diverse etiologies, incidence, prognosis, and survival. HM represents the fourth most common malignancy; approximately 1.29 million people are living with HM. Half of the cases are diagnosed in people over 65 years of age, and 70% of cancer deaths occur in this same population. This group of patients is more vulnerable, which complicates their care. Cognitive impairment, functional dependence, and frailty are frequent factors; they are associated with greater toxicity to treatment. The management of these patients is a challenge due to comorbidities and physiological changes associated with age, which are relationed to the risk of treatment complications. There is little evidence of clinical management guidelines for decision-making in this population. The American Society of Clinical Oncology (ASCO) recommends that all older adults with cancer receiving chemotherapy have a geriatric evaluation. There are recommended evaluation scales, such as the G8 and the geriatric evaluation in hematology (GEH), of which the latter is considered the gold standard. Recent clinical trials suggest that geriatric assessment-guided interventions reduce treatment toxicity, improve quality of life, and improve communication with patients and caregivers. Unfortunately, these trials were conducted on patients with solid tumors.
Aim
Describe the frequency of geriatric evaluation and its value in decision-making regarding chemotherapy treatment in geriatric patients with HM.
Methods:
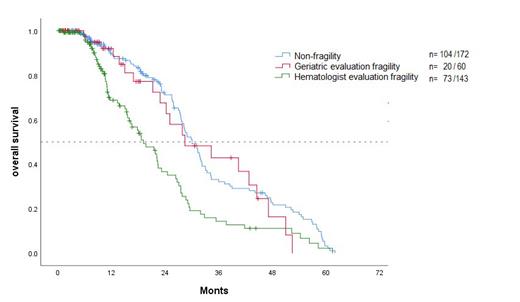
We retrospectively reviewed the data from clinical records of patients with a diagnosis of hematological malignancy aged 65 years or older who have received treatment at the National Institute of Cancerology from 2018 to 2022. An overall survival analysis was performed using the methodology described in the Kaplan - Meier method, looking for differences between groups using the log rank test.
Results:
We analyzed 405 patients with a hematological diagnosis in the elderly; 52 % were women, and the median age at diagnosis was 72 years (range 65-92 years). The diagnoses were non-Hodgkin lymphoma in 71 %, multiple myeloma in 14 %, Hodgkin lymphoma in 6 %, acute leukemia in 4 %, myeloprolipherative neoplasm in 2 %, lymphoproliferative neoplasm in 2.2%, and myelodysplasia neoplasm in 1.5 %. The most prevalent lymphoma corresponds to diffuse large B-cell lymphoma at 66.7 %. All patients (62.4%) with at least one comorbidity. The stratification and risk of hematological diagnosis correspond to advanced and high risk in 74.6 % and 65.4%, respectively.
The frequency of geriatric evaluation was 10.6 % at diagnosis. Considered 15.6 % with fragility for geriatricians, 39 % with fragility for hematologists, and 45.4 % non-fragility. Received intensive chemotherapy in 59 %, adjusted in 34%, and palliative in 4 %. The frequency of treatment modification was 14.8 %, according to the recommendations issued in the geriatric evaluation prior to the start of treatment, which were 4.9%, and modification for the hematologist was 60 %. The frequency of treatment modifications according to the recommendations issued in the geriatric evaluation during treatment is 40 %.
The response was complete in 58%, with 31 % relapse or progression and 10 % partial response. The complications that occurred more frequently were sepsis in 64 % and SARS COV-2 infection in 13 %. Of all patients, 52.5% are alive (follow-up was 60 months), median overall survival (OS) was 27.4 months, and treatment-related mortality (TRM) was 9.4%. Overall survival at 1 year is 82%, at 2 years, 58%, and at 3 years, 27%.
Conclusions:
Assessment geriatric in patients with hematological malignancy is 10.6 %. Intensive chemotherapy is more frequently administered in patients younger than 75 years, but there is no difference in OS with respect to clinical stage, presence of comorbidities, type of chemotherapy (intensive or adjusted), or presence of complications (p ≥ 0,05). OS is better when evaluated by a geriatrician (p = 0,000), for which reason a comprehensive geriatric assessment is considered important for the management of geriatric patients. We recommend that all older adults with cancer receiving chemotherapy have a geriatric evaluation.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal